A German man has remained in HIV remission for over six years following a stem cell transplant initially intended to treat leukemia. This breakthrough, along with recent cases, is reshaping how scientists approach a potential HIV cure, suggesting that complete reliance on rare genetic mutations isn’t necessary.
The Case of Berlin 2
The patient, known as Berlin 2 (B2), received stem cells from a donor carrying one copy of the CCR5 Δ32 mutation – a genetic variation that makes immune cells resistant to HIV. Previously, it was believed that two copies were required for lasting remission. B2 stopped antiretroviral therapy (ART) in 2018 against medical advice and has remained virus-free since.
This challenges the assumption that the mutation must be present in duplicate to prevent HIV from re-establishing itself. The fact that B2’s remission persists with only one mutated CCR5 copy raises critical questions about how durable resistance can be achieved.
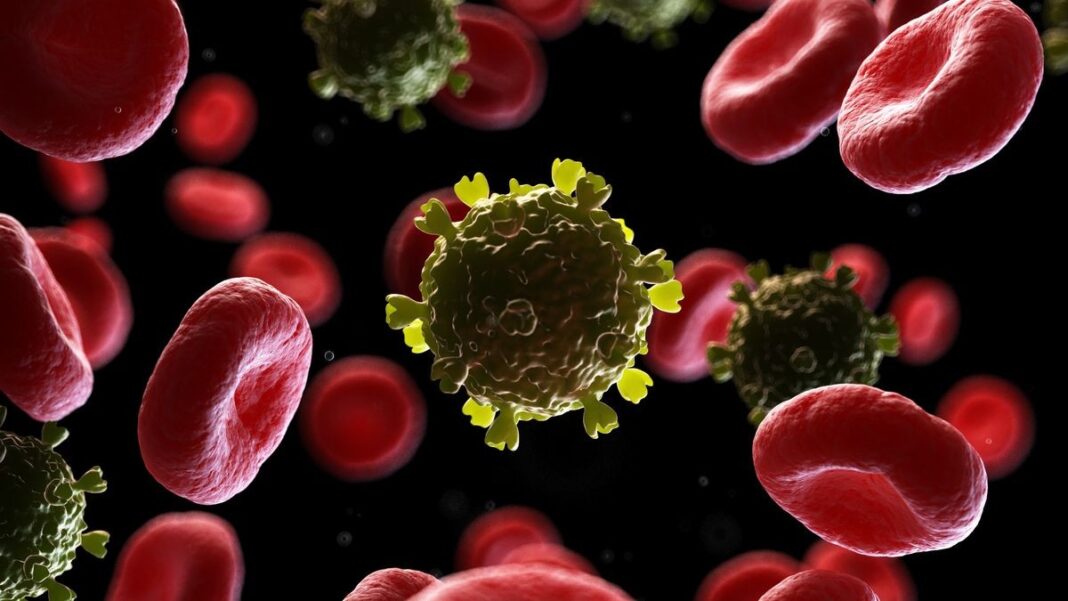
Why HIV is Hard to Treat
HIV is notoriously difficult to eradicate because it integrates its genetic material into the host’s DNA. This creates latent reservoirs of the virus in long-lived immune cells, where it remains hidden from ART, the standard treatment that suppresses viral replication. If ART is stopped, the virus can rebound from these reservoirs.
Stem cell transplants offer a unique solution by aggressively wiping out the existing immune system with chemotherapy, then rebuilding it with donor cells. This process can eliminate viral reservoirs through a phenomenon called graft-versus-reservoir response.
The Role of Stem Cell Transplants
The procedure involves first destroying the patient’s immune system with chemotherapy. Then, donor stem cells are transplanted, which rebuild the immune system from scratch. In some cases, these new cells eliminate remaining HIV reservoirs, leading to long-term remission.
Of the seven known long-term HIV remission cases (Berlin, London, Duesseldorf, New York, City of Hope, and B2), five involved donors with two copies of the CCR5 Δ32 mutation. However, a sixth patient in Geneva achieved remission with a donor who lacked the mutation entirely, suggesting alternative mechanisms can work.
What This Means for Future Treatments
While full stem cell transplants are too risky for widespread HIV treatment, these cases provide critical insights. The focus is shifting towards replicating reservoir depletion, partial CCR5 protection, and the graft-versus-reservoir response through pharmaceutical treatments and gene editing.
Researchers are actively exploring ways to achieve similar results without the severe side effects of a full transplant. The Geneva patient and B2’s cases demonstrate that durable HIV remission isn’t solely dependent on rare genetic mutations.
“Significant reductions of persistent reservoirs can lead to HIV cure independent of homozygous CCR5Δ32-mediated viral resistance,” the researchers conclude. “This underscores the critical importance of modulating and potentially eliminating the HIV reservoir in strategies aimed at long-term remission and cure.”
This research reinforces the possibility of functional HIV cures through innovative therapies that target viral reservoirs directly, rather than relying on genetic luck.